Knowledge Center
Understanding Infertility
General Infertility: Infertility Causes, Testing and Treatment Definition of infertility: 12 months or more of unprotected intercourse without pregnancy
- Primary infertility: Infertility without any previous pregnancy.
- Secondary infertility: Fertility problems occurring in a couple that has conceived on their own and had a child in the past.
- Sterility: When there is no chance for a pregnancy. This is different from infertility which generally represents a reduced potential for pregnancy.
Most childless couples with a female age under about 45 that are having problems getting pregnant are considered to be infertile but not sterile.
When to see a fertility specialist?
- In general, it is appropriate to see a doctor for medical assistance after 12 months of trying to get pregnant on your own.
- Many couples will start the infertility workup process with their general gynecologist, while others prefer to go straight to a fertility specialist. Either option is appropriate.
- It is advised to see a specialist sooner if the female partner is over 35 years old.
It is prudent to seek medical help for fertility issues without waiting for a year of trying on your own if you have a condition that is a known risk factor for fertility problems, such as irregular menstrual cycles, endometriosis, previous tubal pregnancy, PCOS – polycystic ovary syndrome, previous pelvic inflammatory disease (PID), etc.
The appropriate amount of time to try on your own can be longer, or shorter than one year. For example, if you are only 25 years old and feel that you want to give it more time to occur naturally – you might try on your own for another 6 months before seeing a doctor for help.
In 2008, ASRM published a revised definition of infertility that says:
“Infertility is a disease, defined by the failure to achieve a successful pregnancy after 12 months or more of regular unprotected intercourse. Earlier evaluation and treatment may be justified based on medical history and physical findings and is warranted after 6 months for women over age 35 years.”
- For couples with a female partner age 40 or older, it is appropriate to see a fertility specialist if not pregnant by 3-4 months of trying to conceive.
- A high percentage of women over 40 will have age-related issues (egg quality) and will need medical help to get pregnant.
- If the female partner is 42 or older, it is recommended to see a specialist right away if wanting to have a baby.
Fertility advice
You do not need to have sex all the time in order to get pregnant. If you like it that way, then no problem – it doesn’t reduce a couple’s fertility potential either. The best fertility advice in terms of frequency of intercourse is – every day or every other day “around ovulation”.
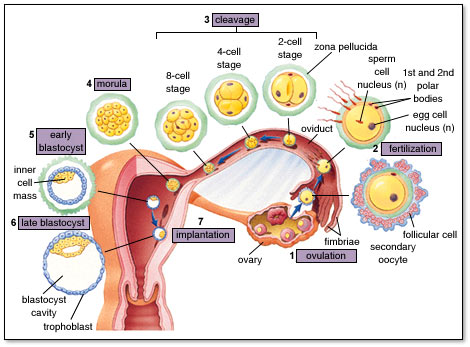
- Ovulation is usually on day 14 – if the menstrual cycle length (from day 1 to day 1) is 28 days, or on day 16 if periods are 30 days apart.
- In other words, ovulation usually occurs 14 days before the next period comes.
The egg only lives about 12-24 hours, while the sperm (if normal) will live in the female’s reproductive tract for up to 2-5 days – while maintaining the ability to fertilize an egg.
- Therefore, the best fertility advice would be to have sex on the day of ovulation, or the day before ovulation (or both).
- Having sex more than about 24 hours after ovulation should be fun and all that, but it isn’t likely to increase the planetary population.
Causes of problems getting pregnant
The cause of infertility is investigated by performing fertility tests in a basic infertility evaluation. The tests can be completed during one menstrual cycle (one month).
What causes infertility? The most common causes are:
- Ovulation problems
- Tubal infertility
- Sperm problems
- Unexplained infertility
- Fertility and female age issues
- Egg quantity and quality problems
Less common causes:
- Uterine problems and infertility
- Infertility and endometriosis
- Previous tubal ligation surgery – tied tubes
- Previous vasectomy surgery

Basic infertility evaluation – fertility tests
History
- The doctor will ask questions to try to get clues as to the cause of yourinfertility.
- These questions will be regarding your medical, surgical, gynecological, and obstetric history, as well as some lifestyle questions.
- A review of records from other fertility doctors that you have seen is also important.
Physical exam
- A directed physical exam that may include a pelvic ultrasound should be performed.
- Ultrasound can help us discover abnormalities with theuterus, fallopian tubes and/or ovaries. We can sometimes see evidence of pelvic scarring, such as when an ovary appears to be stuck to the uterus.
- We get information regarding the woman’s potential for adequate ovarian stimulation with medications by countingantral follicles.
Assessment of ovarian reserve
- This is a very important assessment of a woman’s remaining egg supply
- It is done with blood testing and ultrasound:
- Blood -day 3 FSH, LH and estradiol hormone testing and AMH hormone levels
- Ultrasound – assessment of ovarian volume andantral follicle counts
Assessment of adequate ovulation
This can be done in a variety of ways. About 25% of all infertility is caused by an ovulation disorder. One type of ovulation problem, polycystic ovarian syndrome, is effectively treated with medications.
Semen analysis
The semen analysis is a very important test and should be done early in the evaluation process. If a severe sperm defect is discovered, the testing on the female partner should be modified, and therapy can be immediately directed to the sperm problem.
- About 25% of all infertility is caused by asperm defect and 40-50% of infertility cases have a sperm defect as the main cause, or a contributing cause.
Blood tests
Depending on the individual couple’s situation, various blood tests on either the female or the male may be needed. Blood tests that might be needed include day 3 follicle stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), AMH, prolactin, testosterone (T), progesterone (P4), 17-hydroxyprogesterone (17-OHP), thyroxin (T4), thyroid stimulating hormone (TSH).
If there is a history of recurrent miscarriages (2 or more) a lupus anticoagulant (LAC) and anti-cardiolipin antibody (ACL) are often done, as well as other tests.
Immunological testing has not been proven to have any value in infertility patients without a history of 2 or more miscarriages.
Testing for tubal potency and normalcy of the uterine cavity with a hysterosalpingogram
The hysterosalpingogram, or HSG is done in order to assess the anatomy of the endometrial cavity of the uterus and the fallopian tubes. The HSG is usually scheduled between days 6 and 13 of the cycle – after bleeding and before ovulation.
- This test is usually performed in a radiology facility
- About 25% of all infertility is due to atubal factor
Laparoscopy
- This is a surgical procedure and should not be performed until the basic testing has been done on both partners.
- In some cases,laparoscopy for infertility will be indicated to look for pelvic scarring or endometriosis
- Asin vitro fertilization success rates have improved dramatically over the past 20 years, laparoscopy for infertility is being done much less than before.
- Most couples skip the invasive laparoscopic surgery and do treatments with intrauterine insemination and then IVF if insemination are not successful.
