Female Investigation
Ovarian Reserve Test
This detailed scan is performed to look at the size, shape and condition of the uterus, lining of the womb, both ovaries and the pelvic area. An antral follicle count (also known as an egg sac count) is also performed. An Ovarian Reserve Test (ORT) is a scan carried out between days 1 and days 5 of the menstrual cycle. This scan is best performed transvaginally for optimum clarity.
Hormonal
This is a female screening package which forms part of a basic fertility workup. These tests are best performed between days 1 and 5 of the menstrual cycle.
- FSH
- LH
- E2
- AMH
- Prolactin
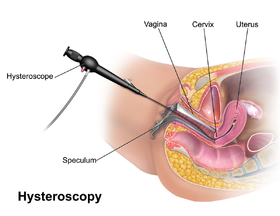
Hysteroscopy
This investigation involves placing a narrow telescope with a camera into the womb and is used to examine the lining of the womb and the opening of the fallopian tubes, to determine whether there are any polyps, fibroids or adhesions present.
Introduction
A hysteroscopy is a procedure used to examine the inside of your uterus using a device called a hysteroscope, which is a narrow telescope with a light and camera at the end, that can easily be passed into your uterus through your vagina and cervix.
The resulting images are sent to a monitor so your consultant can see inside your uterus to locate any problems.
In terms of treatment, your consultant is able to easily diagnose conditions such as fibroids, polyps and Intrauterine adhesions, which can be removed safely during the procedure.
Who?
A hysteroscopy can be used to investigate symptoms and treat problems relating to heavy periods, unusual bleeding, pelvic pain, repeated miscarriages or other likely causes of infertility. It may also be used during a dilatation and curettage procedure or endometrial biopsy to provide a more detailed view of the uterine lining.
How?
We will use a speculum (similar to that used in a smear test) to open your vagina to enable us to pass a hysteroscope through your cervix and into your uterus. We will then gently pump fluid into your uterus to make it easier for us to see the images clearly on a monitor to pinpoint any abnormalities.
What Happens Next ?
The procedure usually takes 20 – 30 minutes in total. Your consultant will discuss the results of the investigations or any treatment performed before you leave the clinic. It is preferable that someone accompanies you home although you should be able to resume your normal activities the following day.
What Are The Side-Effects / Risks?
You may experience slight cramping and some spotting or light bleeding for a few days afterwards. We would recommend you abstain from intercourse for at least one week or until any bleeding has stopped so as to reduce any risk of infection. Whilst a hysteroscopy is generally a very safe procedure, there is a small risk of complications, which is higher for women who have had treatment undertaken during a hysteroscopy. This can include, accidental damage to your uterus or cervix although this is very rare. You may also develop an infection which presents as a fever and heavy bleeding.
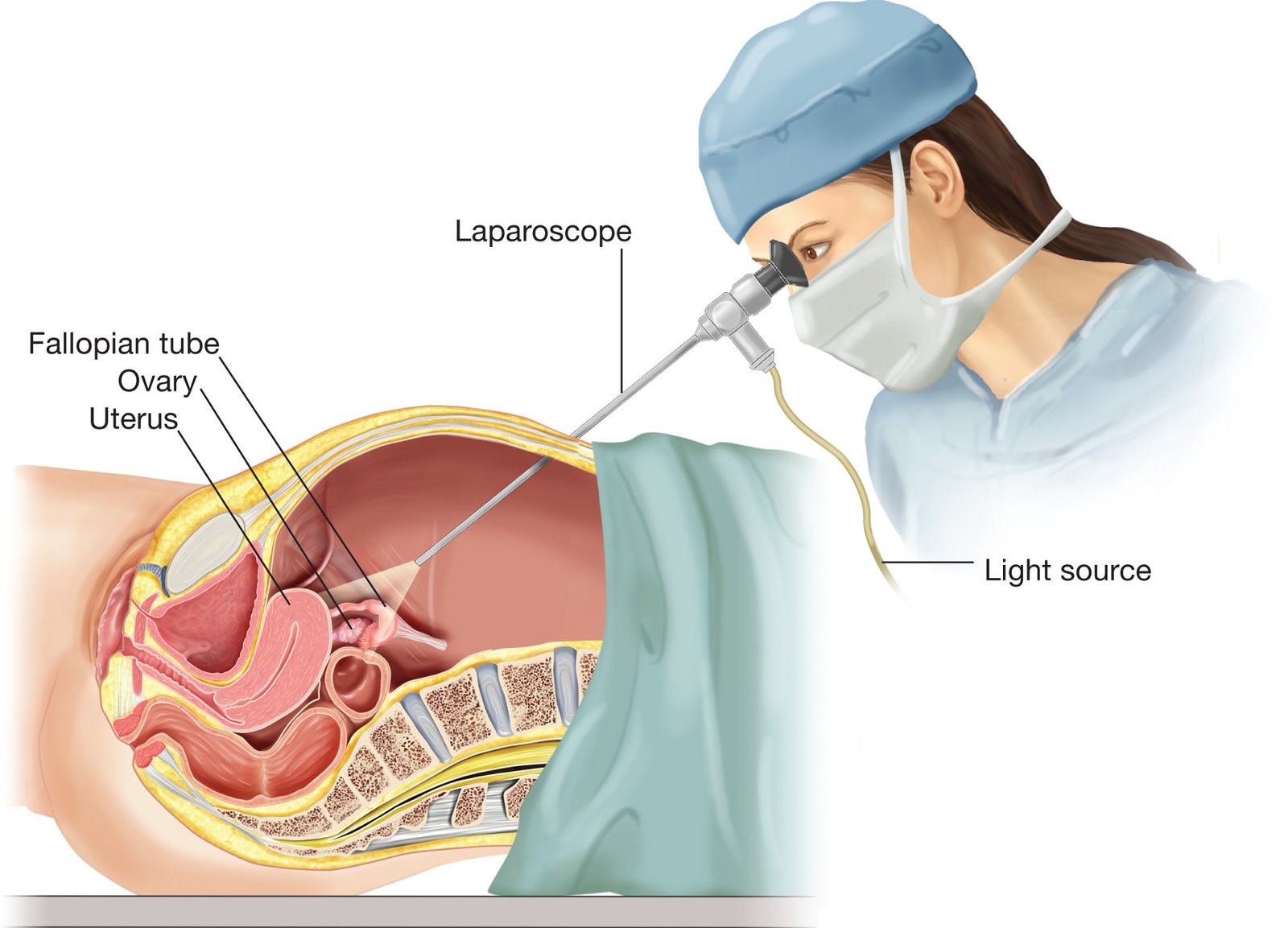
Laparoscopy
During a laparoscopy, a small telescope (laparoscope) is inserted into the abdomen to look directly at the internal tissue to diagnose the presence pelvic pathology eg endometriosis. This test is conducted under a general anaesthetic.
Introduction
Laparoscopy is a keyhole (or minimally invasive) surgical procedure performed under general anaesthetic. It involves inserting a thin fiber-optic telescope fitted with a light and camera through a small incision, usually in the belly button, enabling visualisation of the uterus, fallopian tubes and ovaries. This helps us diagnose and treat any defects such as scar tissue, endometriosis, fibroids or any other abnormalities.
Any abnormalities can be corrected using an operative laparoscopy which involves inserting surgical tools through other small incisions in the lower abdomen, usually at the top of the pubic hair line, which enable the reproductive surgeon to operate from a point of triangulation. This is less invasive than a traditional surgical procedure, leading to a quicker recovery time and reduced scarring.
Who?
A laparoscopy is usually required to assist in the diagnosis and treatment of a wide range of conditions that can develop in the woman’s reproductive organs, including endometriosis, fibroids, polyps, cysts, uterine/pelvic adhesions and blocked fallopian tubes.
How ?
All laparoscopies are conducted under general anaesthetic, so that you will not feel any pain or discomfort throughout the procedure.
Your surgeon will make one or more small incisions in your abdomen through which they can insert the laparoscope and any required surgical tools. They will inflate your abdomen with gas through a tube to make it easier for them to see the areas on which to operate.
When concluded, the gas is released out from your abdomen and the incisions are closed with stitches. The sites will then have a dressing applied and you will be taken to recovery to awaken. Typically the procedure can last between 20 minutes to 2 hours but it may be longer if substantial operative work is required.
What Next?
You will be discharged from the clinic approximately two hours after your surgery and will need to be accompanied home to rest. You will usually need to take off 1-2 days from work. Mild to moderate pain should be anticipated for 7-10 days after the procedure and can be alleviated with over the counter pain relief.
What are the side-effects/risks?
This is a commonly performed procedure and whilst complications are typically rare, minor complications resulting from this surgery can include a post-operative infection or bruising around the incision site(s) and some women may experience feeling sick or tearful after having had a general anaesthetic. There is also the very rare possibility of damage to other organs in the pelvis such as your bowel or bladder or damage to a major artery but this is extremely unusual when a laparoscopy is expertly performed on healthy women.
Dummy Embryo Transfer
This is a procedure which emulates the process of embryo transfer and helps to establish whether an actual transfer is likely to encounter problems. Performed between days 7-12 of the menstrual cycle.
Endometrial Biopsy
This investigation involves the removal of a tiny piece of tissue from the inner lining of the uterus. Performed between days 7-12 of the menstrual cycle.
Endometrial Receptivity Analysis & Timed Embryo Replacement
A lack of synchronisation between the embryo and endometrial receptivity is one of the main causes of recurring implantation failure
Introduction
This procedure is a personalised genetic test that involves taking a biopsy of your womb lining, (the endometrium), to see when it is most receptive for embryo implantation.
Who?
Typically, a lack of synchronisation between the embryo being transferred and your endometrial receptivity is one of the main causes of recurring implantation failure. This is why it is imperative to assess the endometrium in order to determine the optimal day for embryo transfer.
In a normal reproductive cycle, a woman is most receptive to transfer during days 19-21. This is what is known as the ‘window of implantation’. If however, the woman’s cycles are irregular, we need to monitor the endometrium to assess when this optimum time is in order to prepare the embryos in our laboratory for a timed transfer.
How?
You will need to undergo a traditional cycle of IVF treatment in order that we can collect and fertilise your eggs with your partners (or donors) sperm and monitor your developing embryos in our laboratory.
If we have advised that an ERA and timed replacement is necessary, we will freeze your embryos for use at the optimum time in your cycle, conducive with the ERA test results or for a subsequent treatment. The ERA test will have to be done either in a natural cycle or medicated cycle to mimic the type of cycle to be chosen for the actual frozen embryo replacement. So in the event the transfer is to be scheduled in a natural cycle, then the biopsy will be taken 6 days after confirmed ovulation by ultrasound (or 7 days post LH surge). Alternatively, if you have been advised a transfer in a medicated HRT cycle then the biopsy will be taken on the 6th day of progesterone administration.
A biopsy is quickly and easily taken by our consultant in our procedure room. The test will be able to advise whether your endometrium is receptive or non-receptive.
If receptive, this indicates that your window of implantation falls on the day of your cycle during which the biopsy was performed and that an embryo could be transferred to the uterus during this same period in a subsequent frozen embryo transfer cycle following the same regime
What Happens Next?
Once the embryos have been transferred into your uterus, you will be need to continue taking any drugs prescribed in your treatment and wait 16 days before taking a pregnancy test to see if your treatment has been successful. You can continue your day to day activities but we recommend you refrain from any strenuous physical exercise and rest if you feel you need to. The clinic will confirm your pregnancy with ultrasound scans and blood tests before discharging you back to your own GP for antenatal care.
What Are The Side Effects / Risks ?
Pain after this procedure is usually mild but you may experience spotting or light bleeding and your next menstrual period may be early or late. You will be given antibiotics to prevent infection. Infection usually presents as fever, pain in your abdomen or foul-smelling discharge from your vagina.
If at any time you are concerned, please do contact the clinic for advice





 WhatsApp us
WhatsApp us